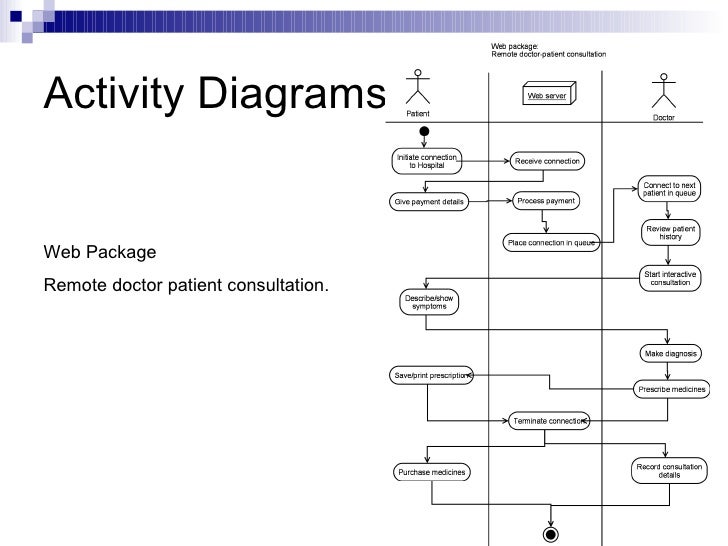
Activity Diagram Doctor
Elements of an Activity Diagrams Activity a behavior that an object carries out while in a particular state Transition – a movement from one activity or state to another Decision point – a diamond symbol containing a condition whose results provide transitions to different paths of activities Synchronization bar – horizontal. The system identifies whether the person is a doctor or staff and handles various activities such as draw salary and give salary, also it adds doctor/staff information into database. This system is responsible for handling various other activities like deleting, editing doctor/staff information into the database. Welcome to My Activity. Data helps make Google services more useful for you. Sign in to review and manage your activity, including things you’ve searched for, websites you’ve visited, and videos you’ve watched. Create a visual plot diagram of Dr. Separate the story into the Exposition, Conflict, Rising Action, Climax, Falling Action, and Resolution. Create an image that represents an important moment or set of events for each of the story components. Write a description of each of the steps in the plot diagram. Lesson Plan Reference.
Affinity Diagram Example
Activity Diagram Doctor Practice
An affinity diagram is the organized output from a brainstorming session. Use it to generate, organize, and consolidate information related to a product, process, complex issue, or problem. After generating ideas, group them according to their affinity, or similarity.
The following example comes from a hospital setting. Seeking to better understand the barriers to on-time delivery of medications, the team created an affinity diagram in six steps.
- Assigned a group leader for the activity.
- Agreed on a statement of the issue or problem.
Tip: Stating the problem in the form of a question (“What are the barriers to on-time delivery of medications?”) can often prove useful. - Brainstormed and recorded ideas.
Tip: You have two main options for gathering ideas from team members. Participation by everyone in the group is assured with silent recording (option b, below), but traditional brainstorming can also generate ideas.- Traditional brainstorming—In order around the group, each person writes an idea or response to the question on a 3” x 5” card while announcing the content of the card to the group.
- Silent recording—Each person writes responses on 3” x 5” cards or sticky notes, one idea per card, until all team members have exhausted their store of ideas.
- Attached all of the cards to the wall, grouping similar ideas together. For example, the team posted together all topics that suggested that the pharmacy may be understaffed.
Tip: After posting all ideas the first time, fine-tune the groupings by moving cards from one pile to another to reflect closer ties. Team members should talk with each other as they arrange the ideas. - Labeled each final grouping with a header identifying the general topic that all items in the group share. See the figure below.
- Reviewed final groupings and headers. By walking around and examining the posted notes, all members of the group had an opportunity to see the groupings and then to comment on them.
Next Steps: Making Connections to Other Tools
While an affinity diagram may present interesting data and useful ideas, the exercise itself should lead to further analysis. The team can now use a relations diagram, for example, or even a cause-and-effect (fishbone) diagram to get to root causes for late medications.
An affinity diagram, above all, stimulates discussion about a problem or issue, opening up possibilities for improvement or solution.
Affinity Diagram: On-time Delivery of Medications
Activity Diagram Online
Contributed by Barbara A. Cleary, vice president, PR and publications,
PQ Systems, Inc.
Activity Diagram Doctor Salary
Adapted from Jacqueline D. Graham and Michael J. Cleary’s Practical Tools for Continuous Improvement, Vol II (Dayton: PQ Systems, Inc., 2002) and Sandra K. Murray and O. Byron Murray’s Practical Tools for Healthcare Quality (Dayton: PQ Systems, Inc., Revised 2009). Used with permission.